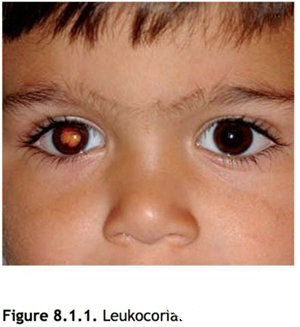
小儿眼科学之白瞳症
【定义】
瞳孔区有白色反光。
【病因学】
1. 视网膜母细胞瘤(Retinoblastoma, Rb) 视网膜恶性肿瘤。
形态上分为三型:
①内生型:瘤体呈白色结节样团块,突向玻璃体生长;
②外生型:瘤体向向我们深层发展,可造成视网膜脱离;
③弥漫浸润型:病变呈弥漫、浸润性生长,可被误诊为葡萄膜炎。
常见虹膜新生血管,可发生假性前房积脓和玻璃体种植。白内障少见,眼球大小正常。
可以是单眼、双眼或多灶性发病。常发生于12~24个月大的婴儿。
大约10%可有家族史。
2. 弓蛔虫病 线虫感染,可表现为视网膜局限的白色隆起的肉芽肿;或是弥漫性眼内炎。
可伴有眼组织的局限性炎症,玻璃体牵引带合并黄斑牵引、牵引性视网膜脱离和白内障。
双眼发病少见,一般发生于6个月~10岁的儿童。
前房穿刺抽取房水检查可见嗜伊红细胞,血清酶联免疫吸附试验(ELISA)弓蛔虫为阳性。
患者可有接触幼犬或不洁饮食史。
3. Coats病
视网膜血管异常,造成小的、多灶性视网膜血管外翻。
白瞳症可继发于渗出性视网膜脱离或广泛的黄色视网膜内和视网膜下渗出。
通常发生于20岁以前的男性,重症病例发生于10岁以前。
Coats病极少双眼发病,没有家族遗传史。

4. 永存增生性原始玻璃体(PHPV)/永存胚胎血管(PFV) 发育性眼部异常,包括不同程度的玻璃体腔内神经胶质和血管增生。
通常合并有轻度的小眼球。
晶状体后纤维膜可对睫状突造成牵拉,病变呈进展状态,伴有生时或生后不久即出现的白内障。晶状体后纤维膜和晶状体可向前推移,使前房变浅,造成继发青光眼。可有视网膜脱离。
多为单眼发病,没有家族遗传史。
5. 先天性白内障 生时出现晶状体混浊,单眼或双眼发病,可有家族遗传史,或伴有全身性疾病。
6. 视网膜星形细胞瘤 无蒂的或轻度隆起的视网膜团块,呈黄白色,可有钙化。通常与结节性硬化症有关,少数与神经纤维瘤有关。
患有结节性硬化的患者可见视神经巨大玻璃膜疣。
7. 早产儿视网膜病变(ROP) 多发于早产儿。
常因视网膜脱离而出现白瞳症。
8. 其他 包括视网膜脉络膜缺损、视网膜脱离、家族性渗出性玻璃体视网膜病变(FEVR)、有髓神经纤维、葡萄膜炎、色素失调征。
【检查】
1. 病史 发病年龄?有无前述疾病的家族史?有无早产?有无幼犬接触史或不洁饮食习惯。
2. 全面的眼科检查 包括角膜直径测量,以观察有无小眼球;检查有无虹膜新生血管、白内障;散瞳查眼底和前部玻璃体。
3. 以下检查有助于明确诊断和确定治疗方案
(1)B型超声 适用于无法窥见眼底的病例。
(2)眼底荧光血管造影适用于Coats病、早产儿视网膜病变、视网膜母细胞瘤。
(3)眼眶及颅脑CT或MRI 适用于视网膜母细胞瘤,尤其是双眼病例或有家族史者,以及晚期Coats病患者。
(4)弓蛔虫血清ELISA试验 大多数弓蛔虫感染病例,滴度1:8时为阳性。
(5)全身检查由小儿科医师对视网膜星形细胞瘤和视网膜母细胞瘤患儿做全身检查。
(6)房水细胞学检查适用于弓蛔虫病。
4. 对于年龄小或不合作的儿童,特别是疑为视网膜母细胞瘤、弓蛔虫病、Coats病或早产儿视网膜病变者,可考虑在麻醉状态下进行检查。
注:对视网膜母细胞瘤患眼做前房穿刺可导致肿瘤细胞扩散。
【治疗】
1. 视网膜母细胞瘤 眼球摘除术,放疗,光凝,化疗,化学复位术,热化疗,有时采用其他方法。全身化疗用于转移癌。
2. 弓蛔虫病
(1)皮质类固醇药物,根据炎症的严重程度,局部滴眼,球周注射或全身用药。
(2)玻璃体切除术:有玻璃体视网膜牵引带形成,或药物治疗无效或恶化时。
(3)如果弓蛔虫可见,行激光光凝。
3. Coats病 激光光凝或冷凝封闭渗漏的血管,手术治疗视网膜脱离,但手术效果欠佳。
4. 永存增生性原始玻璃体
(1)白内障摘除术和手术切除晶状体后神经胶质膜。
(2)治疗弱视。继发于永存增生性原始玻璃体伴发的黄斑发育不良的患者的视力预后通常欠佳。
5. 先天性白内障 参见本章第八节先天性白内障。
6. 视网膜星形细胞瘤 观察。
7. 早产儿视网膜病变 参见本章第二节早产儿视网膜病变。
【随访】
根据诊断而决定。
Definition定义
A white pupillaryreflex
Etiology【病因学】
• Retinoblastoma: Amalignant tumor of the retina that appears as a white, nodular mass extendinginto the vitreous (endophytic), as a mass lesion underlying a retinaldetachment (exophytic), or as a diffusely spreading lesion simulating uveitis(diffuse infiltrating). Iris neovascularization is common. Pseudohypopyon andvitreous seeding may occur. Cataract is uncommon, and the eye is normal insize. May be bilateral, unilateral, or multifocal. Diagnosis is usually madebetween 12 and 24 months of age. A family history may be elicited in about 10%.
• Toxocariasis: A nematode infection that mayappear as a localized, white, elevated granuloma in the retina or as a diffuseendophthalmitis. Associated with localized inflammation of ocular structures,vitreous traction bands and related macular dragging, traction retinaldetachment, and cataract. It is rarely bilateral and is usually diagnosedbetween 6 months and 10 years of age. Paracentesis of the anterior chamber mayreveal eosinophils; serum enzyme-linked immunosorbent assay (ELISA) test forToxocara organisms is positive. The patient may have a history of contact withpuppies or eating dirt.
• Coats disease (see Figure 8.1.2): A retinalvascular abnormality resulting in small multifocal outpouchings of the retinalvessels. Leukocoria may develop secondary to an exudative retinal detachment orto extensive yellow intraretinal and subretinal exudate. Usually develops inboys during the first two decades of life; more severe cases occur in the firstdecade of life. Coats disease is rarely bilateral. No family history.
• Persistent hyperplastic primary vitreous(PHPV)/Persistent fetal vasculature (PFV): A developmental ocular abnormalityconsisting of a varied degree of glial and vascular proliferation in thevitreous cavity. It is usually associated with a slightly small eye. Typicallythere is a membrane behind the lens that may place traction on the ciliaryprocesses. This is a progressive condition with a cataract present at birth orearly in life. The membrane and lens may rotate anteriorly, shallowing theanterior chamber and resulting in secondary glaucoma. Retinal detachments maybe seen. Rarely bilateral. No family history.
• Congenital cataract: Opacity of the lenspresent at birth; may be unilateral or bilateral. There may be a family historyor an associated systemic disorder. See 8.8, Congenital Cataract.
• Retinal astrocytoma: A sessile to slightlyelevated, yellow–white retinal mass that may becalcified and is often associated with tuberous sclerosis, and rarelyneurofibromatosis. May be associated with giant drusen of the optic nerve inpatients with tuberous sclerosis.
• Retinopathy of prematurity (ROP): Predominantlyoccurs in premature children. Leukocoria is usually the result of a retinaldetachment. See 8.2, Retinopathy of Prematurity.
• Others: retinochoroidal coloboma, retinaldetachment, familial exudative vitreoretinopathy (FEVR), myelinated nervefibers, uveitis, incontinentia pigmenti.
Work-Up检查
1 History: Ageat onset? Family history of one of the conditions mentioned? Prematurity?Contact with puppies or habit of eating dirt?
2 Complete ocular examination,including a measurement of corneal diameters (look for a small eye), anexamination of the iris (look for neovascularization), and an inspection of thelens (look for a cataract). A dilated fundus examination and anterior vitreousexamination are essential.
3 Any or all of thefollowing may be helpful in diagnosis and planning treatment:
—B-scan ultrasonography(US), if there is no view of the fundus.
—Intravenous fluoresceinangiogram (Coats disease, ROP, retinoblastoma).
—Computed tomographic(CT) scan or magnetic resonance imaging (MRI) of the orbit and brain(retinoblastoma), particularly for bilateral cases or those with a familyhistory, as well as for cases of advanced Coats disease.
—Serum ELISA test forToxocara (positive at 1:8 in the vast majority of infected patients).
—Systemic examination(retinal astrocytoma, retinoblastoma) by pediatrician.
—Anterior chamberparacentesis (toxocariasis).
4 Consider examination underanesthesia (EUA) in young or uncooperative children, particularly when retinoblastoma,toxocariasis, Coats disease, or ROP is being considered as a diagnosis. See8.8, Congenital Cataract, for a more specific cataract work-up.
(Note
Anterior chamberparacentesis in a patient with a retinoblastoma can possibly lead to tumor celldissemination.
Treatment治疗
1Retinoblastoma: Enucleation, irradiation, photocoagulation, cryotherapy,chemoreduction, chemothermotherapy, or occasionally other therapeuticmodalities. Systemic chemotherapy is used in metastatic disease.
2 Toxocariasis:
—Steroids (topical,periocular, or systemic routes may be used, depending on the severity of theinflammation).
—Consider a surgicalvitrectomy when vitreoretinal traction bands form or when the condition doesnot improve or worsens with medical therapy.
—Consider laserphotocoagulation of the nematode if it is visible.
3 Coats disease:Laser photocoagulation or cryotherapy to leaking vessels. Though associatedwith a poor outcome, surgery may be required for a retinal detachment.
4 PHPV:
—Cataract and retrolentalglial membrane extraction.
—Treat any amblyopia,though visual outcome is often poor secondary to foveal hypoplasia associatedwith PHPV.
5 Congenitalcataract: See 8.8, Congenital Cataract.
6 Retinalastrocytoma: Observation.
7 ROP: See 8.2,Retinopathy of Prematurity.
Follow-Up随访
Variable, dependingon the diagnosis.